Evidence-based personalized rehabilitation protocols for uneventful healing with datadriven virtual twins
PIs: Benedikt Braun, Michael Roland, Annchristin Andres, Stefan Diebels
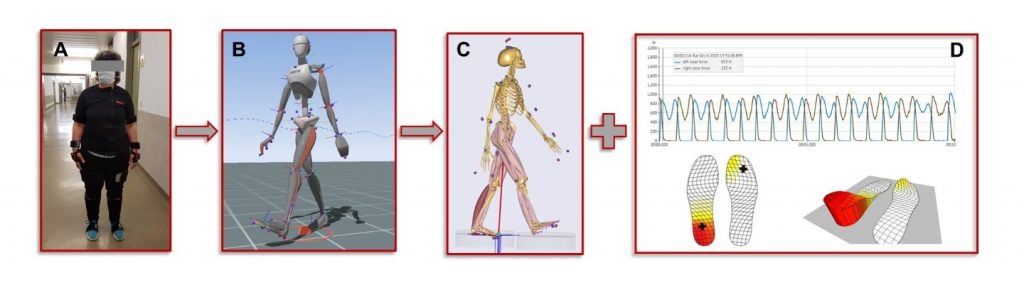
Illustration of the motion capturing workflow: A) patient wearing the motion capturing system and the insoles, B) avatar of the motion capturing analysis software, C) representation of the musculoskeletal model scaled with the patients‘ body measurements and equipped with the motion data, D) typical result of the sensor insole during gait.
Aim:
The collaboration tackles the challenge of extending fracture healing to a multi-X computational model via virtual twin technology based on patient-specific clinical trial data over the course of healing during rehabilitation.
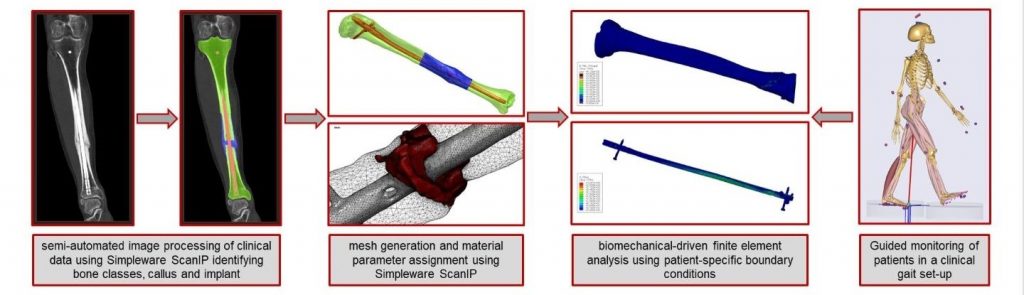
Illustration of the workflow from clinical imaging via segmentation and model generation to personalized biomechanical finite element analysis based on patient-specific monitoring data.
Description:
Fracture healing is a complex, multi-faceted process influenced by various mechanical and biological factors. However, conventional rehabilitation protocols are often based on a one-size-fits-all approach that ignores individual patient differences and can lead to suboptimal healing outcomes. By creating a virtual twin for each patient, this project aims to close this gap. The virtual twin will link real-time data from body-worn sensors with musculoskeletal simulations and provide constraints for patient-specific computer models to simulate the healing process – from the macro-level biomechanics of the bone-implant system to the micro-level cellular activities and mechanobiology.
The project’s main goal is to develop and establish an innovative digital process chain for the realization of virtual twins of patients with lower extremity fractures to enable an individualized treatment and follow-up process that improves the current standard rehabilitation structure with its persistently high complication rates. Therefore, the virtual twin will be designed with a holistic approach combining a wide range of measurement technologies, data analytics, modeling, and simulation concepts to represent a healing fracture’s entire patient-specific life cycle. We hypothesize that the virtual twin will enable a personalized healing prognosis at an early postoperative time point, referred to as the trajectory of healing at t=0, virtually mapping the further rehabilitation process. The data collected at later points in time make the virtual twin dynamic, and the ongoing simulations and data analyses transform it into a kind of living system that describes the patient’s healing process in a highly individualized way.
The project is divided into six work packages covering the spectrum, from clinical data collection to wearable sensors (WP1) and clinical validation (WP6). The digital process chain and the resulting virtual twin (WP2) connect all work packages and the different levels of the multi-X fracture healing model. In WP5, the image processing and, thus, the geometric 3D model creation are realized, while in WP4, the movement analysis and the musculoskeletal simulation take place. The core of the virtual twin is the multi-X healing model to be implemented in WP3, which is intended to predict the healing process based on the data from the other work packages.
Involved Institutions:
Chair of Applied Mechanics, Saarland University, Saarbrücken, Germany
Department of Trauma and Reconstructive Surgery, Eberhard-Karls-University Tuebingen, BG Unfallklinik, Tuebingen, Germany
Links:
Applicants:

Prof. (apl.) Dr. med. Benedikt Braun

Dr. rer. nat. Michael Roland

Prof. Dr.-Ing. Stefan Diebels

Annchristin Andres, M. Sc.
Publications
2024
Braun, Benedikt J; Histing, Tina; Menger, Maximilian M; Herath, Steven C; Mueller-Franzes, Gustav A; Grimm, Bernd; Marmor, Meir T; Truhn, Daniel
In: Injury, Bd. 55, Nr. 2, 2024, ISSN: 0020-1383.
@article{Braun2024,
title = {Wearable activity data can predict functional recovery after musculoskeletal injury: Feasibility of a machine learning approach},
author = {Benedikt J Braun and Tina Histing and Maximilian M Menger and Steven C Herath and Gustav A Mueller-Franzes and Bernd Grimm and Meir T Marmor and Daniel Truhn},
doi = {10.1016/j.injury.2023.111254},
issn = {0020-1383},
year = {2024},
date = {2024-02-00},
urldate = {2024-02-00},
journal = {Injury},
volume = {55},
number = {2},
publisher = {Elsevier BV},
keywords = {},
pubstate = {published},
tppubtype = {article}
}
2023
Roland, Michael; Diebels, Stefan; Orth, Marcel; Pohlemann, Tim; Bouillon, Bertil; Tjardes, Thorsten
In: Sci Rep, Bd. 13, Nr. 1, 2023, ISSN: 2045-2322.
@article{Roland2023,
title = {Reappraisal of clinical trauma trials: the critical impact of anthropometric parameters on fracture gap micro-mechanics—observations from a simulation-based study},
author = {Michael Roland and Stefan Diebels and Marcel Orth and Tim Pohlemann and Bertil Bouillon and Thorsten Tjardes},
doi = {10.1038/s41598-023-47910-2},
issn = {2045-2322},
year = {2023},
date = {2023-12-00},
urldate = {2023-12-00},
journal = {Sci Rep},
volume = {13},
number = {1},
publisher = {Springer Science and Business Media LLC},
abstract = {<jats:title>Abstract</jats:title><jats:p>The evidence base of surgical fracture care is extremely sparse with only few sound RCTs available. It is hypothesized that anthropometric factors relevantly influence mechanical conditions in the fracture gap, thereby interfering with the mechanoinduction of fracture healing. Development of a finite element model of a tibia fracture, which is the basis of an in silico population (n = 300) by systematic variation of anthropometric parameters. Simulations of the stance phase and correlation between anthropometric parameters and the mechanical stimulus in the fracture gap. Analysis of the influence of anthropometric parameters on statistical dispersion between in silico trial cohorts with respect to the probability to generate two, with respect to anthropometric parameters statistically different trial cohorts, given the same power assumptions. The mechanical impact in the fracture gap correlates with anthropometric parameters; confirming the hypothesis that anthropometric factors are a relevant entity. On a cohort level simulation of a fracture trial showed that given an adequate power the principle of randomization successfully levels out the impact of anthropometric factors. From a clinical perspective these group sizes are difficult to achieve, especially when considering that the trials takes advantage of a „laboratory approach “, i.e. the fracture type has not been varied, such that in real world trials the cohort size have to be even larger to level out the different configurations of fractures gaps. Anthropometric parameters have a significant impact on the fracture gap mechanics. The cohort sizes necessary to level out this effect are difficult or unrealistic to achieve in RCTs, which is the reason for sparse evidence in orthotrauma. New approaches to clinical trials taking advantage of modelling and simulation techniques need to be developed and explored.</jats:p>},
keywords = {},
pubstate = {published},
tppubtype = {article}
}
Orth, Marcel; Ganse, Bergita; Andres, Annchristin; Wickert, Kerstin; Warmerdam, Elke; Müller, Max; Diebels, Stefan; Roland, Michael; Pohlemann, Tim
In: Front. Bioeng. Biotechnol., Bd. 11, 2023, ISSN: 2296-4185.
@article{Orth2023,
title = {Simulation-based prediction of bone healing and treatment recommendations for lower leg fractures: Effects of motion, weight-bearing and fibular mechanics},
author = {Marcel Orth and Bergita Ganse and Annchristin Andres and Kerstin Wickert and Elke Warmerdam and Max Müller and Stefan Diebels and Michael Roland and Tim Pohlemann},
doi = {10.3389/fbioe.2023.1067845},
issn = {2296-4185},
year = {2023},
date = {2023-02-20},
urldate = {2023-02-20},
journal = {Front. Bioeng. Biotechnol.},
volume = {11},
publisher = {Frontiers Media SA},
abstract = {<jats:p>Despite recent experimental and clinical progress in the treatment of tibial and fibular fractures, in clinical practice rates of delayed bone healing and non-union remain high. The aim of this study was to simulate and compare different mechanical conditions after lower leg fractures to assess the effects of postoperative motion, weight-bearing restrictions and fibular mechanics on the strain distribution and the clinical course. Based on the computed tomography (CT) data set of a real clinical case with a distal diaphyseal tibial fracture, a proximal and a distal fibular fracture, finite element simulations were run. Early postoperative motion data, recorded <jats:italic>via</jats:italic> an inertial measuring unit system and pressure insoles were recorded and processed to study strain. The simulations were used to compute interfragmentary strain and the von Mises stress distribution of the intramedullary nail for different treatments of the fibula, as well as several walking velocities (1.0 km/h; 1.5 km/h; 2.0 km/h) and levels of weight-bearing restriction. The simulation of the real treatment was compared to the clinical course. The results show that a high postoperative walking speed was associated with higher loads in the fracture zone. In addition, a larger number of areas in the fracture gap with forces that exceeded beneficial mechanical properties longer was observed. Moreover, the simulations showed that surgical treatment of the distal fibular fracture had an impact on the healing course, whereas the proximal fibular fracture barely mattered. Weight-bearing restrictions were beneficial in reducing excessive mechanical conditions, while it is known that it is difficult for patients to adhere to partial weight-bearing recommendations. In conclusion, it is likely that motion, weight bearing and fibular mechanics influence the biomechanical milieu in the fracture gap. Simulations may improve decisions on the choice and location of surgical implants, as well as give recommendations for loading in the postoperative course of the individual patient.</jats:p>},
keywords = {},
pubstate = {published},
tppubtype = {article}
}
Braun, Benedikt J.; Histing, Tina; Menger, Maximilian M.; Platte, Julian; Grimm, Bernd; Hanflik, Andrew M.; Richter, Peter H.; Sivananthan, Sureshan; Yarboro, Seth R.; Gueorguiev, Boyko; Pokhvashchev, Dmitry; Marmor, Meir T.
“Bring Your Own Device”—A New Approach to Wearable Outcome Assessment in Trauma Artikel
In: Medicina, Bd. 59, Nr. 2, 2023, ISSN: 1648-9144.
@article{Braun2023,
title = {“Bring Your Own Device”—A New Approach to Wearable Outcome Assessment in Trauma},
author = {Benedikt J. Braun and Tina Histing and Maximilian M. Menger and Julian Platte and Bernd Grimm and Andrew M. Hanflik and Peter H. Richter and Sureshan Sivananthan and Seth R. Yarboro and Boyko Gueorguiev and Dmitry Pokhvashchev and Meir T. Marmor},
doi = {10.3390/medicina59020403},
issn = {1648-9144},
year = {2023},
date = {2023-02-00},
urldate = {2023-02-00},
journal = {Medicina},
volume = {59},
number = {2},
publisher = {MDPI AG},
abstract = {<jats:p>Background and Objectives: Outcome data from wearable devices are increasingly used in both research and clinics. Traditionally, a dedicated device is chosen for a given study or clinical application to collect outcome data as soon as the patient is included in a study or undergoes a procedure. The current study introduces a new measurement strategy, whereby patients’ own devices are utilized, allowing for both a pre-injury baseline measure and ability to show achievable results. Materials and Methods: Patients with a pre-existing musculoskeletal injury of the upper and lower extremity were included in this exploratory, proof-of-concept study. They were followed up for a minimum of 6 weeks after injury, and their wearable outcome data (from a smartphone and/or a body-worn sensor) were continuously acquired during this period. A descriptive analysis of the screening characteristics and the observed and achievable outcome patterns was performed. Results: A total of 432 patients was continuously screened for the study, and their screening was analyzed. The highest success rate for successful inclusion was in younger patients. Forty-eight patients were included in the analysis. The most prevalent outcome was step count. Three distinctive activity data patterns were observed: patients recovering, patients with slow or no recovery, and patients needing additional measures to determine treatment outcomes. Conclusions: Measuring outcomes in trauma patients with the Bring Your Own Device (BYOD) strategy is feasible. With this approach, patients were able to provide continuous activity data without any dedicated equipment given to them. The measurement technique is especially suited to particular patient groups. Our study’s screening log and inclusion characteristics can help inform future studies wishing to employ the BYOD design.</jats:p>},
keywords = {},
pubstate = {published},
tppubtype = {article}
}
2022
Braun, Benedikt J.; Histing, Tina; Herath, Steven C.; Rollmann, Mika F. R.; Reumann, Marie; Menger, Maximilian M.; Springer, Fabian; Andres, Annchristin; Diebels, Stefan; Roland, Michael
In: Unfallchirurgie, Bd. 125, Nr. 8, S. 619–627, 2022, ISSN: 2731-703X.
@article{Braun2022,
title = {Bewegungsanalyse und muskuloskeletale Simulation in der Pseudarthrosentherapie – Erfahrungen und erste klinische Ergebnisse},
author = {Benedikt J. Braun and Tina Histing and Steven C. Herath and Mika F. R. Rollmann and Marie Reumann and Maximilian M. Menger and Fabian Springer and Annchristin Andres and Stefan Diebels and Michael Roland},
doi = {10.1007/s00113-022-01208-6},
issn = {2731-703X},
year = {2022},
date = {2022-08-00},
urldate = {2022-08-00},
journal = {Unfallchirurgie},
volume = {125},
number = {8},
pages = {619--627},
publisher = {Springer Science and Business Media LLC},
keywords = {},
pubstate = {published},
tppubtype = {article}
}
Ganse, Bergita; Orth, Marcel; Roland, Michael; Diebels, Stefan; Motzki, Paul; Seelecke, Stefan; Kirsch, Susanne-Marie; Welsch, Felix; Andres, Annchristin; Wickert, Kerstin; Braun, Benedikt J; Pohlemann, Tim
Concepts and clinical aspects of active implants for the treatment of bone fractures Artikel
In: Acta Biomaterialia, Bd. 146, S. 1–9, 2022, ISSN: 1742-7061.
@article{Ganse2022,
title = {Concepts and clinical aspects of active implants for the treatment of bone fractures},
author = {Bergita Ganse and Marcel Orth and Michael Roland and Stefan Diebels and Paul Motzki and Stefan Seelecke and Susanne-Marie Kirsch and Felix Welsch and Annchristin Andres and Kerstin Wickert and Benedikt J Braun and Tim Pohlemann},
doi = {10.1016/j.actbio.2022.05.001},
issn = {1742-7061},
year = {2022},
date = {2022-07-00},
urldate = {2022-07-00},
journal = {Acta Biomaterialia},
volume = {146},
pages = {1--9},
publisher = {Elsevier BV},
keywords = {},
pubstate = {published},
tppubtype = {article}
}
2021
Braun, Benedikt J.; Orth, Marcel; Diebels, Stefan; Wickert, Kerstin; Andres, Annchristin; Gawlitza, Joshua; Bücker, Arno; Pohlemann, Tim; Roland, Michael
In: Front. Surg., Bd. 8, 2021, ISSN: 2296-875X.
@article{Braun2021,
title = {Individualized Determination of the Mechanical Fracture Environment After Tibial Exchange Nailing—A Simulation-Based Feasibility Study},
author = {Benedikt J. Braun and Marcel Orth and Stefan Diebels and Kerstin Wickert and Annchristin Andres and Joshua Gawlitza and Arno Bücker and Tim Pohlemann and Michael Roland},
doi = {10.3389/fsurg.2021.749209},
issn = {2296-875X},
year = {2021},
date = {2021-09-29},
urldate = {2021-09-29},
journal = {Front. Surg.},
volume = {8},
publisher = {Frontiers Media SA},
abstract = {<jats:p>Non-union rate after tibial fractures remains high. Apart from largely uncontrollable biologic, injury, and patient-specific factors, the mechanical fracture environment is a key determinant of healing. Our aim was to establish a patient-specific simulation workflow to determine the mechanical fracture environment and allow for an estimation of its healing potential. In a referred patient with failed nail-osteosynthesis after tibial-shaft fracture exchange nailing was performed. Post-operative CT-scans were used to construct a three-dimensional model of the treatment situation in an image processing and computer-aided design system. Resulting forces, computed in a simulation-driven workflow based on patient monitoring and motion capturing were used to simulate the mechanical fracture environment before and after exchange nailing. Implant stresses for the initial and revision situation, as well as interfragmentary movement, resulting hydrostatic, and octahedral shear strain were calculated and compared to the clinical course. The simulation model was able to adequately predict hardware stresses in the initial situation where mechanical implant failure occurred. Furthermore, hydrostatic and octahedral shear strain of the revision situation were calculated to be within published healing boundaries—accordingly the fracture healed uneventfully. Our workflow is able to determine the mechanical environment of a fracture fixation, calculate implant stresses, interfragmentary movement, and the resulting strain. Critical mechanical boundary conditions for fracture healing can be determined in relation to individual loading parameters. Based on this individualized treatment recommendations during the early post-operative phase in lower leg fractures are possible in order to prevent implant failure and non-union development.</jats:p>},
keywords = {},
pubstate = {published},
tppubtype = {article}
}
2020
Braun, Benedikt J.; Grimm, Bernd; Hanflik, Andrew M.; Marmor, Meir T.; Richter, Peter H.; Sands, Andrew K.; Sivananthan, Sureshan
Finding NEEMO: towards organizing smart digital solutions in orthopaedic trauma surgery Artikel
In: EFORT Open Reviews, Bd. 5, Nr. 7, S. 408–420, 2020, ISSN: 2058-5241.
@article{Braun2020,
title = {Finding NEEMO: towards organizing smart digital solutions in orthopaedic trauma surgery},
author = {Benedikt J. Braun and Bernd Grimm and Andrew M. Hanflik and Meir T. Marmor and Peter H. Richter and Andrew K. Sands and Sureshan Sivananthan},
doi = {10.1302/2058-5241.5.200021},
issn = {2058-5241},
year = {2020},
date = {2020-07-00},
urldate = {2020-07-00},
journal = {EFORT Open Reviews},
volume = {5},
number = {7},
pages = {408--420},
publisher = {Bioscientifica},
abstract = {<jats:p> There are many digital solutions which assist the orthopaedic trauma surgeon. This already broad field is rapidly expanding, making a complete overview of the existing solutions difficult. The AO Foundation has established a task force to address the need for an overview of digital solutions in the field of orthopaedic trauma surgery. Areas of new technology which will help the surgeon gain a greater understanding of these possible solutions are reviewed. We propose a categorization of the current needs in orthopaedic trauma surgery matched with available or potential digital solutions, and provide a narrative overview of this broad topic, including the needs, solutions and basic rules to ensure adequate use in orthopaedic trauma surgery. We seek to make this field more accessible, allowing for technological solutions to be clearly matched to trauma surgeons’ needs. </jats:p><jats:p> Cite this article: EFORT Open Rev 2020;5:408-420. DOI: 10.1302/2058-5241.5.200021 </jats:p>},
keywords = {},
pubstate = {published},
tppubtype = {article}
}
2019
Braun, Benedikt J.; Pohlemann, Tim; Herath, Steven C.; Klein, Moritz; Rollmann, Mika F.; Derr, Ralf; Diebels, Stefan; Roland, Michael
In: Arch Appl Mech, Bd. 89, Nr. 11, S. 2351–2360, 2019, ISSN: 1432-0681.
@article{Braun2019,
title = {An individualized simulation model based on continuous, independent, ground force measurements after intramedullary stabilization of a tibia fracture},
author = {Benedikt J. Braun and Tim Pohlemann and Steven C. Herath and Moritz Klein and Mika F. Rollmann and Ralf Derr and Stefan Diebels and Michael Roland},
doi = {10.1007/s00419-019-01582-5},
issn = {1432-0681},
year = {2019},
date = {2019-11-00},
urldate = {2019-11-00},
journal = {Arch Appl Mech},
volume = {89},
number = {11},
pages = {2351--2360},
publisher = {Springer Science and Business Media LLC},
keywords = {},
pubstate = {published},
tppubtype = {article}
}
Braun, Benedikt J; Osche, David; Rollmann, Mika; Orth, Marcel; Mörsdorf, Philipp; Histing, Tina; Pohlemann, Tim; Herath, Steven C
In: Injury, Bd. 50, Nr. 7, S. 1329–1332, 2019, ISSN: 0020-1383.
@article{Braun2019b,
title = {Increased therapy demand and impending loss of previous residence status after proximal femur fractures can be determined by continuous gait analysis – A clinical feasibility study},
author = {Benedikt J Braun and David Osche and Mika Rollmann and Marcel Orth and Philipp Mörsdorf and Tina Histing and Tim Pohlemann and Steven C Herath},
doi = {10.1016/j.injury.2019.05.007},
issn = {0020-1383},
year = {2019},
date = {2019-07-00},
urldate = {2019-07-00},
journal = {Injury},
volume = {50},
number = {7},
pages = {1329--1332},
publisher = {Elsevier BV},
keywords = {},
pubstate = {published},
tppubtype = {article}
}
